
from an article from CNN by Leslie Saxon M.D.
When it comes to digital health products, the prevailing attitude among physicians is still deep suspicion. While many people look at physicians as the drivers of change in digital health, I am in the minority of innovators in this field. There are some physicians who are on the vanguard of talking about it, but only a few are actual innovators. Many of the advances will come from non-healthcare innovators–the “pull through” demand will come from the public who recognize the benefits of new technology to help them become healthier and smarter about their lives.
It is ironic but technology has taken me back to my patients, who are the reason I entered medicine so many years ago. Just as digital technology has enabled us to stay connected to others, it has helped me connect more immediately with my patients. For the patients there is more control as well. Just as we control our finances, our schedules, our travel plans, and music selections through technology we can have greater control over our health and our care.
Technology will always be second to Patient Care. Patients will remain central to all of reform. Physicians, hospitals, and other health care providers must make this their compass.
The fact is that Life with a capital L—my patients’ real, authentic experiences—mostly happen outside of my office. How can I make better observations? How can I—a highly trained person with 25 years of experience—take my knowledge and help more people? Or, help my patients at a deeper level? How can I be a better witness to their story, edit it, and make it better? There are new answers and we hold them in the palms of our hands.
Technologic advances don’t happen in isolation. There are many different elements— cultural and technologic — that must come together to turn an innovation into a scalable business product, and then, possibly—but rarely—a cultural phenomenon.
The internet, for example, changed banking, journalism, and commerce in many parts of the world. But the connection, information, and convenience it afforded missed medicine because the innovation and the cultural desire hadn’t yet arrived. Advancing technologies will soon radically change healthcare. The cultural and technologic pieces are coming together like a rising storm. I remember, like it was yesterday, when we hosted our first University of Southern California Body Computing Conference. It was in 2007.
I wanted to bring together various experts, from Academy Award winners to engineers, to imagine the future of healthcare in a digital world. In several instances, people left in a huff, or laughed off the notion of digital technology changing healthcare. Many of the physician-attendees said the change wouldn’t happen “for two decades.”
The reactions interested me because, in my experience, where there is anger, there is also fear and irrationality.
Just this week Congressional hearings debated digital medicine because lawmakers and regulators recognize that there are hundreds of millions of dollars—including the $10 million Tricorder X Prize—being invested in new, consumer-oriented technology. And these products will soon start hitting the market. At this point, some of the products are more marketing fluff than reality, while others are too difficult to use.
But there is a realization that consumers want, and need, products to connect them with their physicians, their medical records, and with relatives who are helping to manage their care. Mobile phones and other ubiquitous devices are becoming so advanced that the technology within them can be turned into a “health device.” Having changed music and communication, consumer device makers are looking for new revenue streams and they are identifying health as a way to create new revenue streams, and the result will be a change in medicine, which has been working from a 2,000 year old paternalistic doctor-patient model. Guided by Apple Computer Inc., digital technology changed the music industry. Why not change medicine?
When it comes to digital health products, the prevailing attitude among physicians is still deep suspicion. While many people look at physicians as the drivers of change in digital health, I am in the minority of innovators in this field. There are some physicians who are on the vanguard of talking about it, but only a few are actual innovators. Many of the advances will come from non-healthcare innovators–the “pull through” demand will come from the public who recognize the benefits of new technology to help them become healthier and smarter about their lives.
Shortly after the first USC Body Computing Conference, I started a center at the University of Southern California to study and create health solutions. We study digital health by evaluating products in clinical and non-clinical settings, as well as create a variety of solutions, including health games. Calling myself an innovator still feels pretentious. True innovation is really difficult. Being in the innovation trenches has taught me many lessons and given me new respect for the world’s innovators. Being creative and bringing different expertise together is difficult but critical in digital health. We work with different innovators, athletes, engineers, story-tellers and others because health is an all-encompassing issue that a physician alone cannot solve. Working with many of the smartest people in this field, as well as bringing “creative” into medicine, has given me a more holistic view. Being around so many “creative types”—and being exposed to soon-to-be-released technology has also given me special insight into the way the world will look in the near future:
1. Body worn sensors that can transmit your heart rate, blood pressure, brain waves, and other vital signs. Physicians will be looking at this data, and calling you to check in with your specialist;
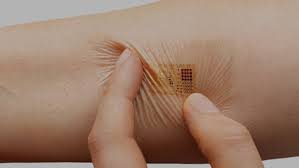
2. Medical content that is of high quality and accurate and specific to you. Currently, medical content is generalized and not very compelling. (We did a study at USC that showed that many popular medical sites have inaccurate information.) Several companies are working on how to “mash up” different bio statistics. It may seem unusual for you to record your every heart beat today, but it might not be too farfetched for your children. Soon there will be inexpensive, tattoo-like sensors that will record information and filter it through analytics—without relying on highly subjective information;
3. New applications that help patients with chronic diseases manage their care, lab results, multiple physicians and medication, and reward patients. A major issue in medicine is compliance. As a physician, I can only get a snapshot of your life, but if I can learn more about you, and if you can help learn yourself, we will be better partners in your care. Eventually, with the information that we learn, we can spend our resources more wisely. There are a lot of promises around Big Data: there are a lot of smart people working on ways to capture and design smart analytics to sift through terabytes of data that could impact millions, if not billions, of people.
Even in the most developing of countries, mobile technology is pervasive. An example of what this could mean: just last year, I was sitting at home. Someone was using a smart phone ECG on the other side of the world. I diagnosed a Nigerian, traveling in Mumbai, who had a heart condition. I can use my unique knowledge and training to help more people, not just my patients in Los Angeles.
There will be people who read these predictions and dismiss them. What about reimbursements? What about FDA regulations? Won’t insurance companies use this information negatively? Won’t there just be medical white noise?
The questions are valid, and they need to be asked. It is always easy to over-simplify and get caught up in the hype. But—as I have learned from other innovators—demanding simplification can return fascinating results. There is a good lesson in the music industry, which stood by helplessly as their industry changed during the digital revolution. There is rapid change happening, and it’s how we address it early, and use the technology to help people, that will dictate our children’s lives. Saying it won’t happen just shows willful blindness.
I welcome the questions. But I’m optimistic. I see the innovation first hand. As a physician, I can see the possibilities for good.
Helping patients deal with the emotions that come with health issues is a large part of the "art" of doctoring. People see their lives and their health as a story. Since that first Body Computing Conference in 2007, I have spent more time with storytellers, especially my colleagues at USC’s School of Cinematic Arts. I have learned a lot about the power of story, of how the story of our lives is in many ways a health narrative.
It is ironic but technology has taken me back to patients, who are the reason I entered medicine so many years ago. Just as digital technology has enabled us to stay connected to others, it has helped me connect more immediately with my patients. For the patients there is more control as well. Just as we control our finances, our schedules, our travel plans, and music selections through technology we can have greater control over our health and our care.
The fact is that Life with a capital L—my patients’ real, authentic experiences—mostly happen outside of my office. How can I make better observations? How can I—a highly trained person with 25 years of experience—take my knowledge and help more people? Or, help my patients at a deeper level? How can I be a better witness to their story, edit it, and make it better? There are new answers and we hold them in the palms of our hands.
Technorati Tags:
mobile apps,
mhealth,
wifi,
wireless health,
connectivity,
patients,
technology,
patient driven,
patient care,
body computing,
body sensors,
medical content,
reimbursement,
congress,
usc computing center,
story teller