Wearable sensors to monitor everything from step count to heart rate are nearly ubiquitous. But for scenarios such as measuring the onset of frailty in older adults, promptly diagnosing deadly diseases, testing the efficacy of new drugs or tracking the performance of professional athletes, medical-grade devices are needed.
University of Arizona engineers have developed a type of wearable they call a "biosymbiotic device," which has several unprecedented benefits. Not only are the devices custom 3D-printed and based on body scans of wearers, but they can operate continuously using a combination of wireless power transfer and compact energy storage. The team, led by Philipp Gutruf, assistant professor of biomedical engineering and Craig M. Berge Faculty Fellow in the College of Engineering, published its findings today in the journal Science Advances.
Current wearable sensors face various limitations. Smartwatches, for example, need to be charged, and they can only gather limited amounts of data due to their placement on the wrist. By using 3D scans of a wearer's body, which can be gathered via methods including MRIs, CT scans and even carefully combined smartphone images, Gutruf and his team can 3D-print custom-fitted devices that wrap around various body parts. Think a virtually unnoticeable, lightweight, breathable, mesh cuff designed specifically for your bicep, calf or torso. The ability to specialize sensor placement allows researchers to measure physiological parameters they otherwise couldn't.
Because these biosymbiotic devices are custom fitted to the wearer, they're also highly sensitive. Gutruf's team tested the device's ability to monitor parameters including temperature and strain while a person jumped, walked on a treadmill and used a rowing machine. In the rowing machine test, subjects wore multiple devices, tracking exercise intensity and the way muscles deformed with fine detail. The devices were accurate enough to detect body temperature changes induced by walking up a single flight of stairs.
Brain Devices
The technology can also be used to analyze brain physiology. The brain presents several challenges. It is behind the blood-brain barrier that prevents many substances, and medications from entering the brain fluid. The mechanism is poorly understood. Some sensory devices involve drilling a hole in the skull and implant a micro sensor with multiple needles that enter the brain with minimal damage to the cortex. However this in itself creates artifacts in signals. -
Current optogenetics experiments, done in animal models, involve introducing a light-sensitive protein, which attaches to specific neurons in the brain. (delivered by viral vectors). A light stimulus is delivered to the brain with an LED under the skin or even of the surface of the skin.
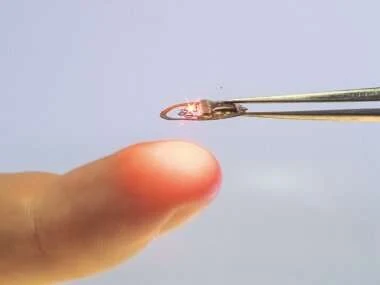 |
| Light emitting diode |
The discussion of opsins goes beyond this blog I recommend reading the references at the end of the article. It is not light reading.
Optogenetic interrogation of neural circuits: technology for probing mammalian brain structures




No comments:
Post a Comment